In the early 20th century, as the world faced one of the deadliest pandemics in history, people turned to all sorts of creative and desperate measures to protect themselves from the flu.
From camphor bags worn around the neck to saltwater gargles and makeshift masks, the fear of the unknown drove both medical professionals and everyday individuals to seek any possible solution.
These eerie and haunting vintage photos capture how the world battled an invisible enemy long before modern vaccines and treatments were available.
The surprising origin of the Spanish Flu name

The term “Spanish flu” is actually a misnomer that originated during World War I. Unlike many European countries involved in the war, Spain was neutral and didn’t censor its press.
Countries like France, England, and the United States imposed wartime censorship, which largely suppressed news about a dangerous virus spreading through troops.
Since Spanish journalists were some of the few reporting on the widespread flu in the spring of 1918, the pandemic became known as the “Spanish flu,” even though Spain was not the origin.
In the summer of 1918, reported cases of the flu decreased. However, by August, a new, mutated strain of the flu emerged somewhere in Europe, capable of killing even healthy individuals within 24 hours of infection.
By late August, military ships left the English city of Plymouth, unknowingly carrying soldiers infected with this deadlier strain.
As these ships reached cities like Brest in France, Boston in the U.S., and Freetown in West Africa, the pandemic’s second and more devastating wave began.

Historian James Harris from Ohio State University explains that the rapid movement of soldiers during World War I played a significant role in spreading the disease.
“The entire military-industrial complex of moving lots of men and material in crowded conditions was certainly a huge contributing factor in the ways the pandemic spread,” Harris notes.
The staggering death toll

Between September and November of 1918, the death toll from the Spanish flu surged dramatically. In the United States alone, October saw 195,000 deaths.
Unlike typical seasonal flu, which predominantly affects the very young and elderly, the second wave of the Spanish flu followed a “W curve.”
This curve showed high mortality rates among the young and old but also an unusual spike in the deaths of healthy adults between the ages of 25 and 35—individuals in the prime of life.
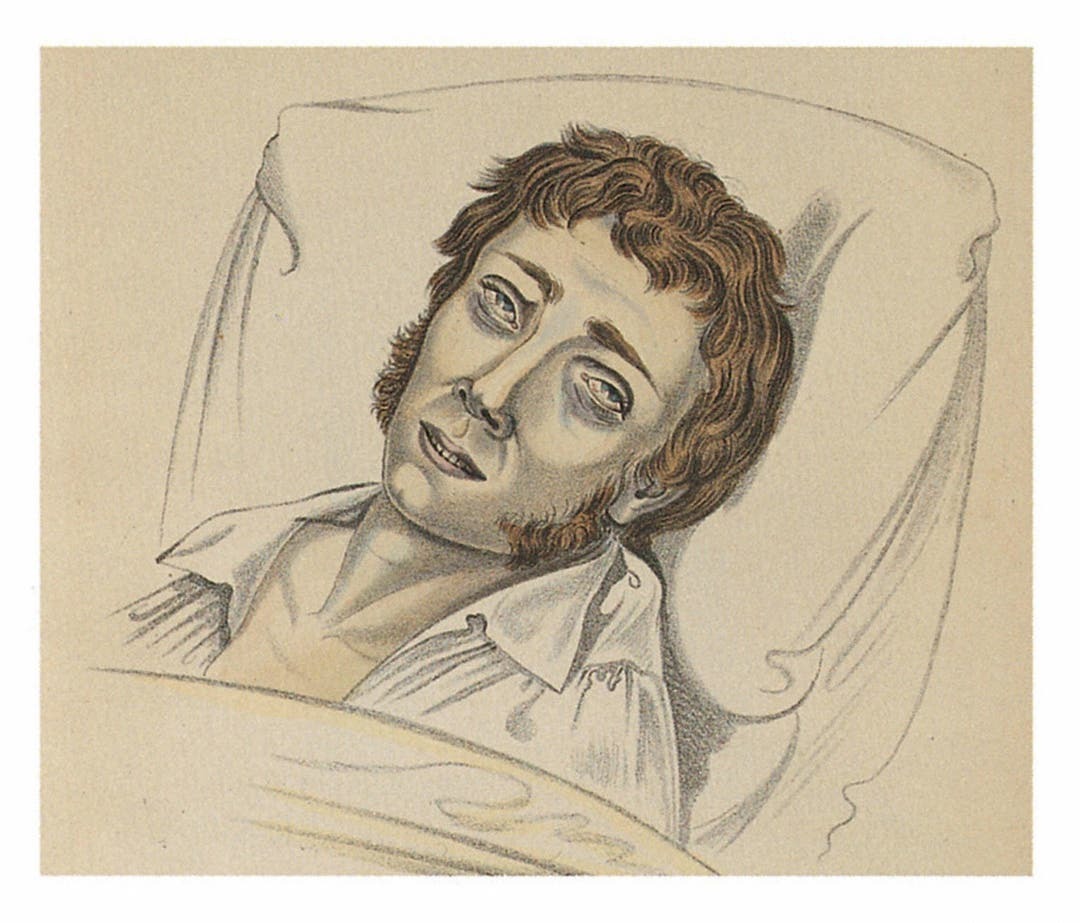
“That really freaked out the medical establishment, that there was this atypical spike in the middle of the W,” says historian James Harris.
It wasn’t just the fact that so many young, healthy people were dying; it was the way they died. Patients suffered from intense fevers, nasal bleeding, and pneumonia, eventually drowning as their lungs filled with fluid.
Decades later, scientists identified the cause behind this deadly phenomenon as a “cytokine storm.” Normally, the immune system releases cytokines to promote inflammation when the body is under viral attack.
However, the H1N1 strain of the Spanish flu triggered an extreme immune response in otherwise healthy individuals, leading to severe inflammation and fluid buildup in the lungs. This overreaction of the immune system proved fatal for many.
British military doctors who performed autopsies on soldiers affected by the second wave noted that the damage to their lungs resembled injuries caused by chemical warfare.
What made flu to spread and grow
Historian James Harris argues that the rapid spread of the Spanish flu in the fall of 1918 was partly due to public health officials’ reluctance to impose quarantines during wartime.
In Britain, Arthur Newsholme, a government official, recognized that a strict lockdown would be the most effective way to prevent the flu’s spread.
However, he chose not to implement such measures because of the fear it would cripple the war effort by keeping munitions workers and other civilians at home.

Newsholme believed that “the relentless needs of warfare justified incurring [the] risk of spreading infection,” encouraging citizens to “carry on” despite the pandemic.
In the United States, a severe nursing shortage weakened the public health response. Many nurses were deployed to military camps and battlefronts, and the situation worsened when the American Red Cross initially refused to employ trained African American nurses.
However, one of the main reasons for the high death toll from the Spanish flu was the lack of scientific knowledge at the time.
Medical science was unable to develop a vaccine, as microscopes in 1918 were not advanced enough to see viruses, which wouldn’t be visible until the 1930s.
At the time, many believed that the flu was caused by a bacterium known as “Pfeiffer’s bacillus.” After a flu outbreak in 1890, German physician Richard Pfeiffer discovered that his patients carried a bacterium he named “H. influenzae.”
When the Spanish flu struck, scientists focused on finding a cure for this bacterium, pouring millions of dollars into laboratories to develop tests and treatments for “H. influenzae” —but it was all in vain.
“This was a huge distraction for medical science,” Harris emphasized how the mistaken focus on bacteria delayed progress in fighting the actual viral cause of the pandemic.
When and how the deadly pandemic ended
By December 1918, the devastating second wave of the Spanish flu had subsided, but the pandemic was far from over. A third wave began in Australia in January 1919 and gradually spread to Europe and the United States.
Even prominent figures weren’t immune—President Woodrow Wilson fell seriously ill with flu-like symptoms in April 1919 while attending the peace negotiations in Paris.
The White House downplayed the severity of his illness and attributed it to a simple cold from Paris’s rainy weather. Wilson eventually recovered and returned to the U.S. in July.
The third wave proved just as lethal as the second in terms of mortality rate. However, the end of World War I meant that the conditions that had fueled the virus’s rapid spread—crowded troop movements and war-related travel—were no longer present.
Although the third wave still claimed millions of lives globally, the losses were not as catastrophic as those during the second wave.

In the early 20th century, people tried various methods to protect themselves from the flu. One common remedy was camphor, extracted from “Cinnamomum camphora” trees.
Many believed that wearing a bag of camphor around the neck would ward off the virus. Doctors and nurses even went as far as injecting it into patients’ arms and legs.
Today, camphor remains in use, notably as an ingredient in “Vicks VapoRub,” though it’s now regulated by the FDA in much smaller, safer doses.
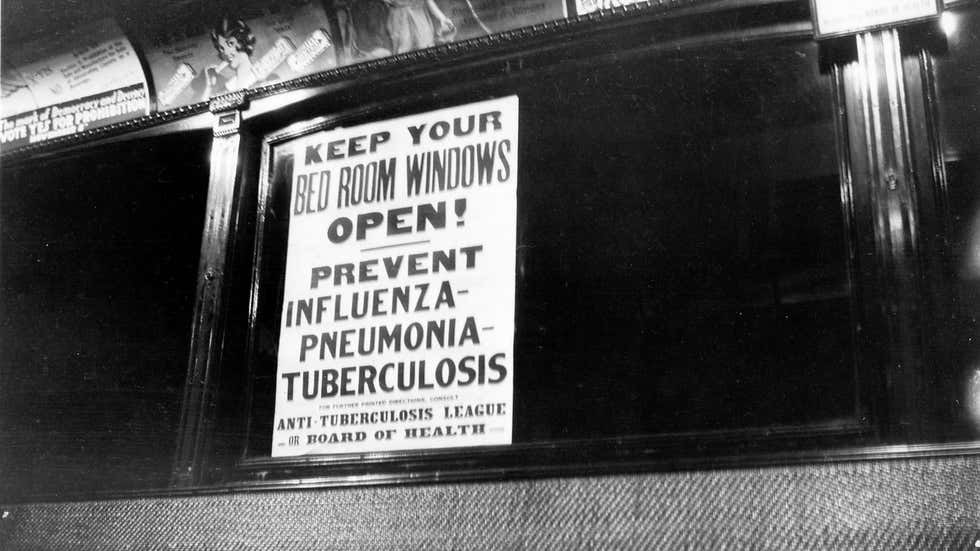
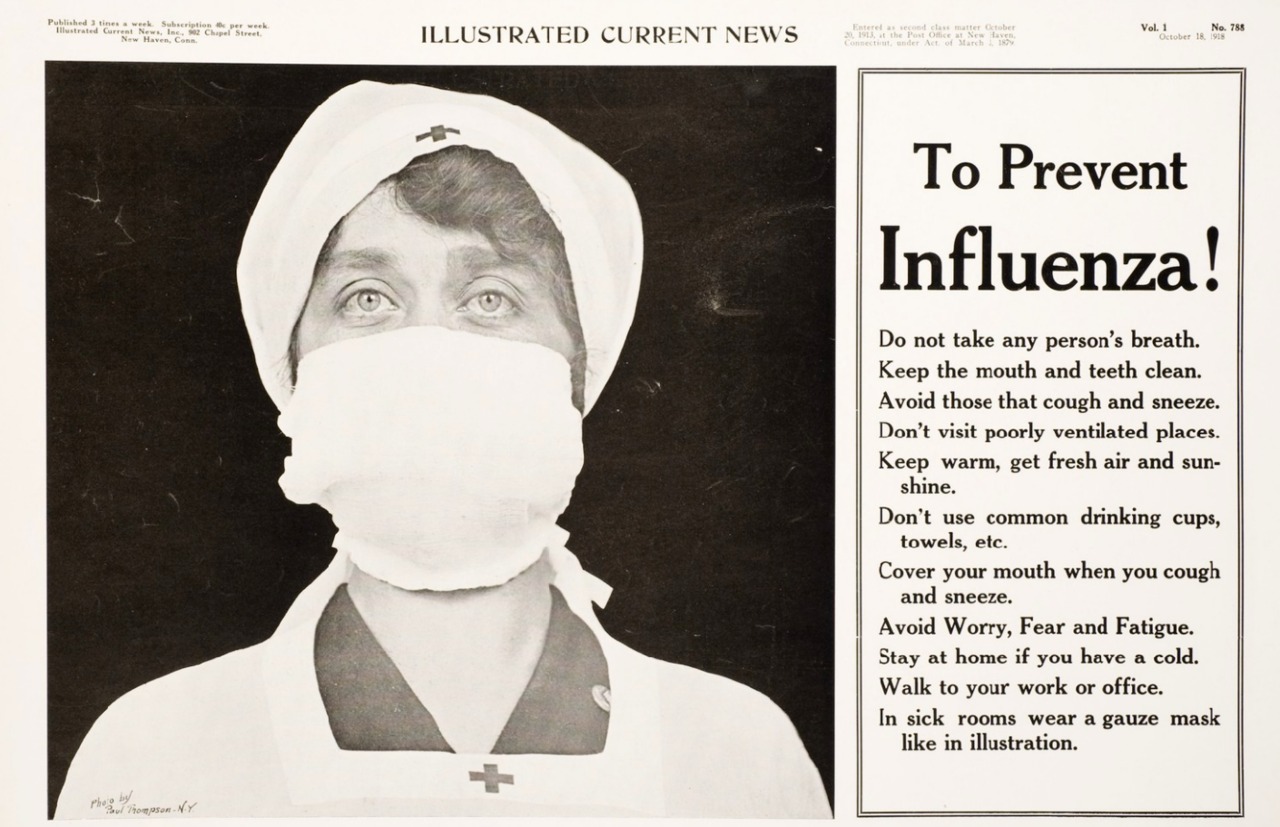
Other protective measures at the time included gargling saltwater, wearing masks, eating oranges, and even discouraging people from kissing babies.
While these habits can still be helpful, the CDC emphasizes that getting an annual flu vaccine is one of the most effective ways to prevent the virus today.
Eerie vintage photos of people battling the flu
1. Cats need flu medicine too

In this picture, two vets are giving a cat named Tibbles anti-flu tablets. Judging by the look on the cat’s face, he might want to change his name to Must-bite-your-fingers Tibbles.
2. Group gargling at school

At Tollgate School, a group of boys performs a gargling routine to prevent the flu. Like their uniforms, the rules and routines, such as gargling, help keep them safe and neat.
3. Daily gargling for flu prevention
 A school nurse gives anti-flu medicine to students, who find it both gross and funny as one of their classmates struggles to take it.
A school nurse gives anti-flu medicine to students, who find it both gross and funny as one of their classmates struggles to take it.
4. Sailors against sickness
 At the Nautical School in Somerset, young cadets were trained to become sailors and were also taught flu prevention techniques. They seem quite happy and proud while following these measures.
At the Nautical School in Somerset, young cadets were trained to become sailors and were also taught flu prevention techniques. They seem quite happy and proud while following these measures.
5. Drink up

During the 1932 flu season, a nurse visited the Mutual Property Insurance Co. in London, teaching staff flu prevention methods with paper cups and pills, even if they weren’t very eco-friendly.
6. Spritz and Go

Two dressed-up actresses are spraying anti-flu tonics into their mouths. Without the bottles, it could easily be mistaken for them singing a duet about the silliness of feathered hats.
7. Business as usual
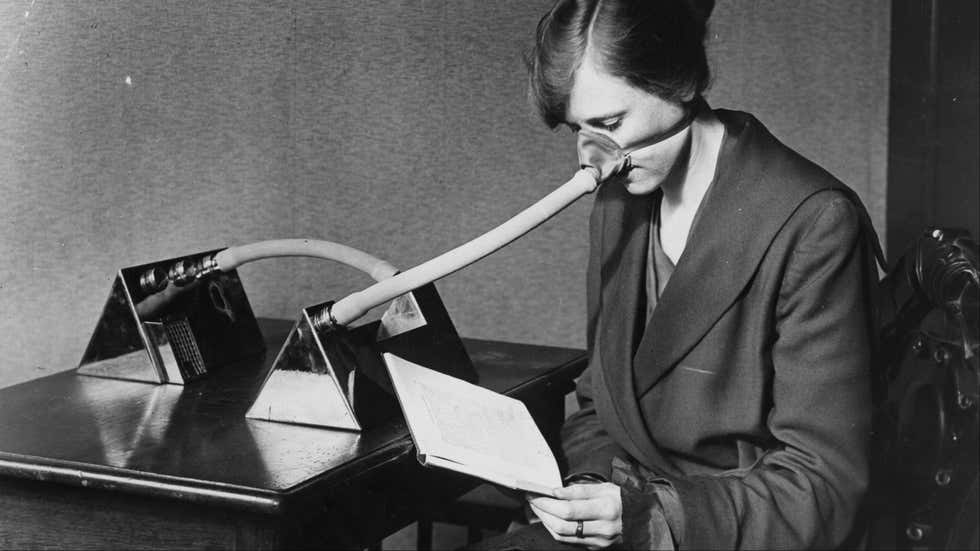
During the 1918 flu epidemic, this woman went about her daily tasks, dressed in a nice jacket, and read an important document. She’s also wearing a strange-looking flu mask that resembles a toilet plunger.
8. Old pros at gargling
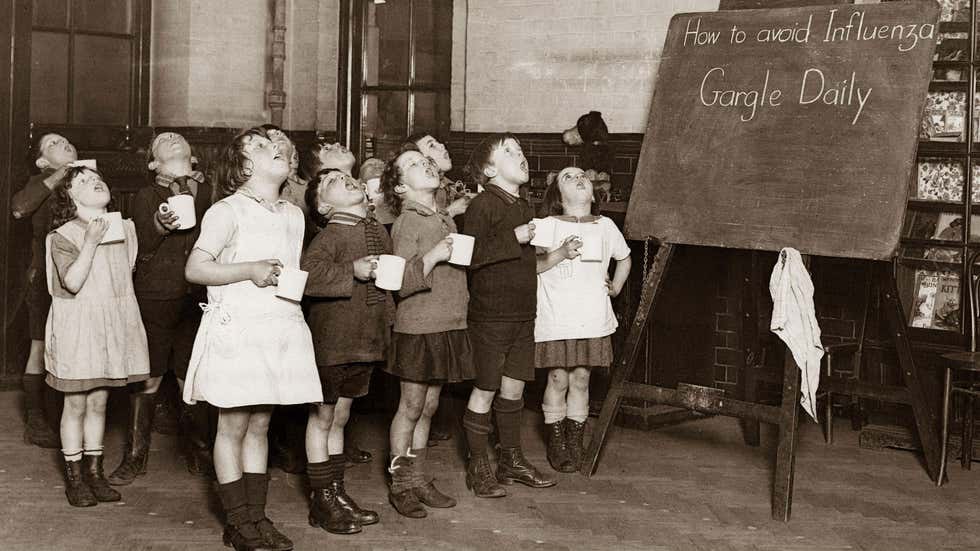
In this 1935 school in England, students were taught to gargle daily from a young age. They seem healthy, so maybe the advice written on the chalkboard worked.
9. Drink ale to cure the flu

In 1937, people believed that mulled ale could prevent the flu. In this photo, an employee is happily serving the drink for free to customers at Thames House.
10. ‘I’m Adorable, But Please Don’t Kiss Me’

In this 1939 photo, the parents had the right idea. Since the flu can spread up to six feet, and babies are at high risk for serious complications, it’s best for unvaccinated individuals to keep their distance.
11. People in England wear different-looking masks to prevent the flu circa 1932.

During a tough flu outbreak in London’s freezing winters of the 1930s, this fashionable couple strolls the streets wearing matching antiseptic masks, showing they can make flu protection look stylish.
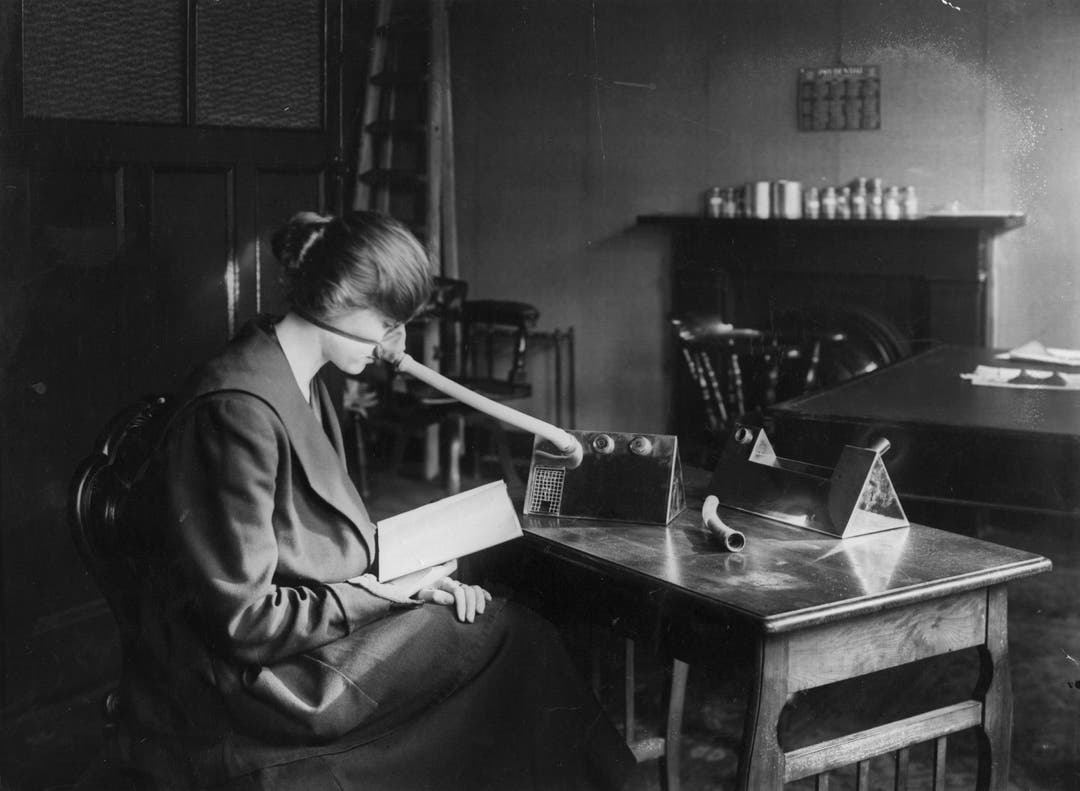
12. Professor Bordier of France’s University of Lyon, with his machine
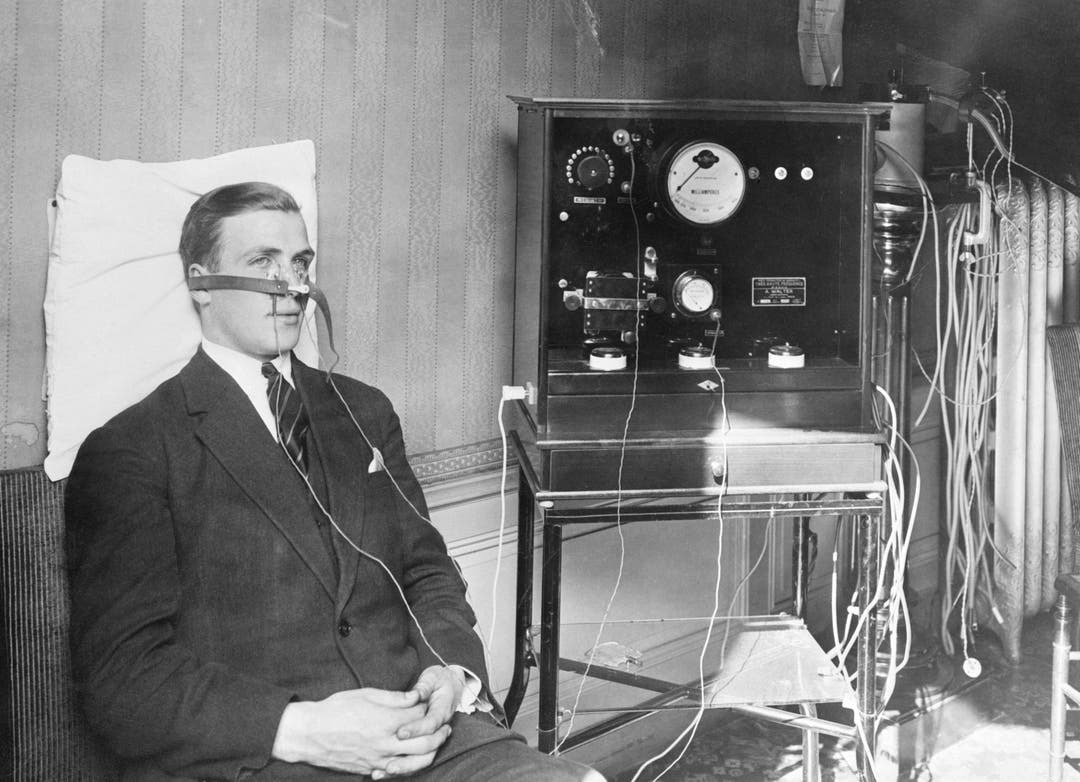
In this 1928 photo, Professor Bordier of France’s University of Lyon demonstrates a machine he claimed could cure colds in minutes.
13. Londoners wearing masks

In this 1932 photo, people in London wear masks to prevent catching the flu—a precaution still commonly used worldwide today.
14. Get your oranges here

In 1940 London, officials believed three oranges a day could help fight off the flu. Here, an officer gives actress Molly Lamont her emergency ration of oranges after a flu outbreak claimed 200 lives at Elstree Studios.
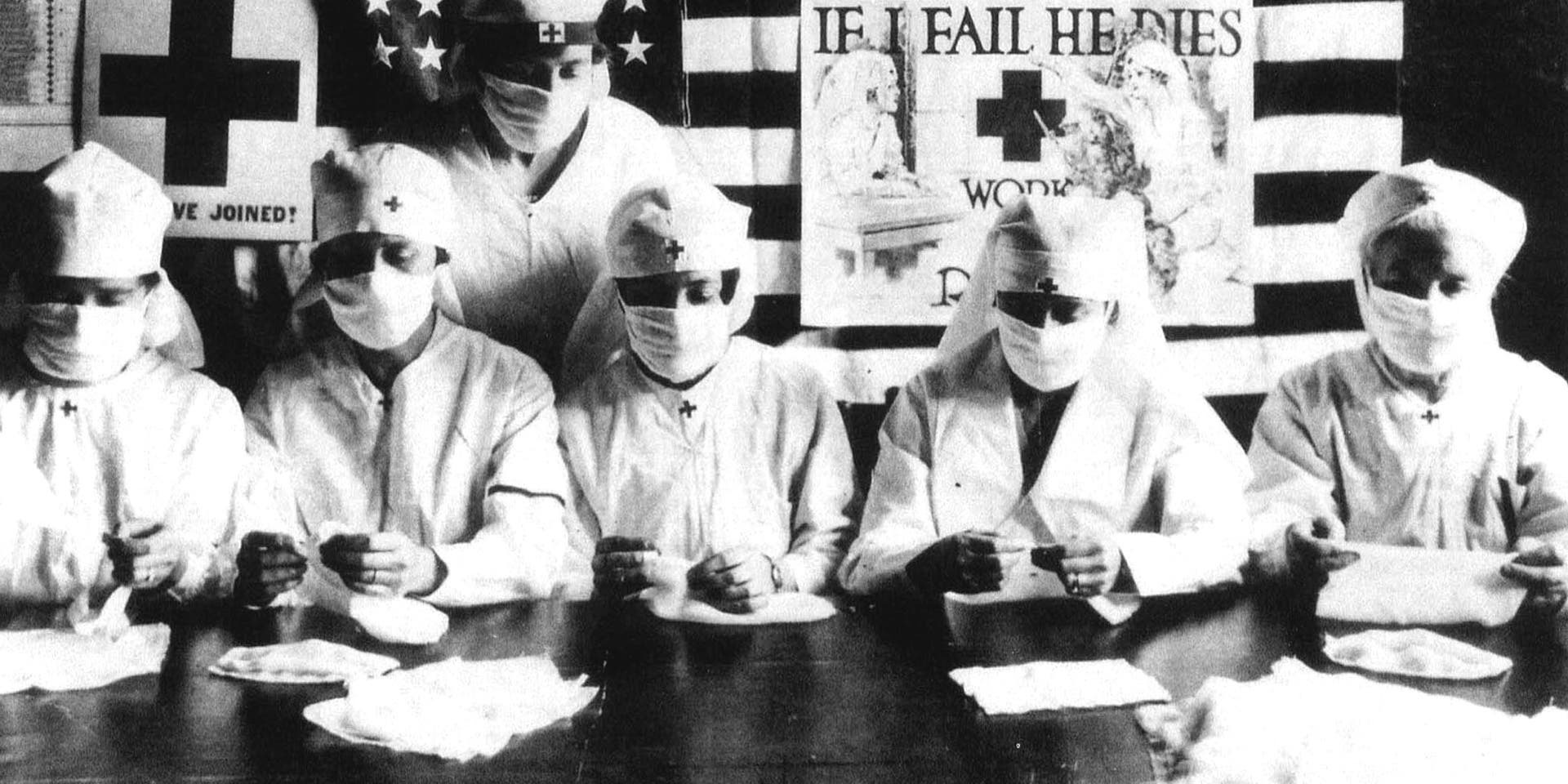
15. Red Cross Volunteers – Boston, MA

During the 1918 flu pandemic, Massachusetts faced a shortage of medical staff as many were called to military service. Governor McCall urged everyone with medical training to help. In Boston, Red Cross volunteers made gauze masks for Camp Devens, one of the hardest-hit areas.
16. Nurse Advertisement – Chicago, IL
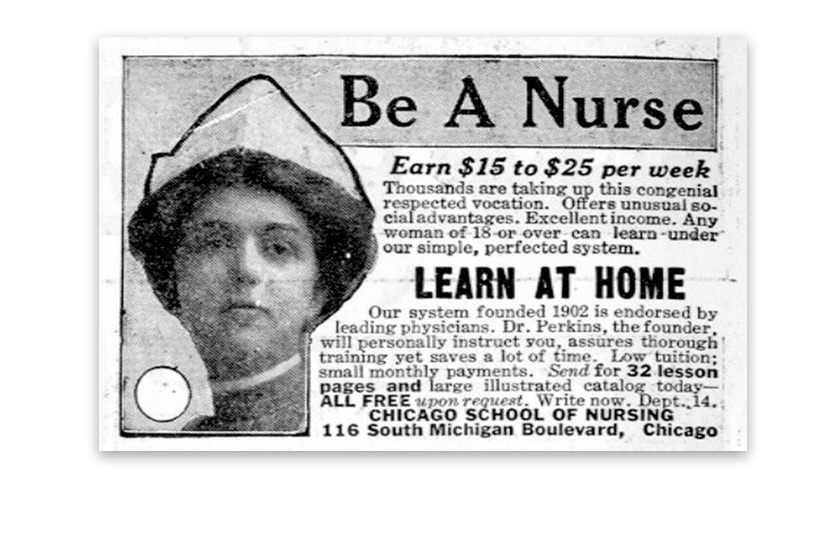
Nurses were in high demand during the epidemic. Advertisements like this one from the Chicago School of Nursing encouraged people to train as nurses to meet the urgent need.
17. Local Barber – Cincinnati, OH
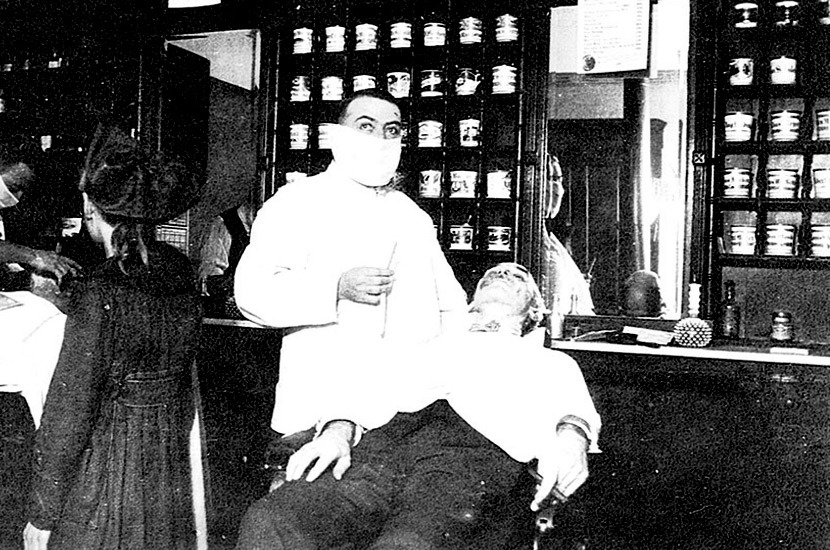
In Cincinnati, barbers and hotel workers were advised to wear masks to help prevent the spread of influenza. This barber wears a mask while giving a shave to a customer.
18. Red Cross Ambulance Demonstration – Washington, DC

As the epidemic worsened, the Red Cross in Washington, DC held a demonstration at an emergency ambulance station. Desperate for help, the Red Cross called for both trained nurses and untrained volunteers to assist. Congress approved a $1 million budget to recruit doctors and nurses.
19. Pharmacist at People’s Drug Store No. 5 – Washington, D.C.
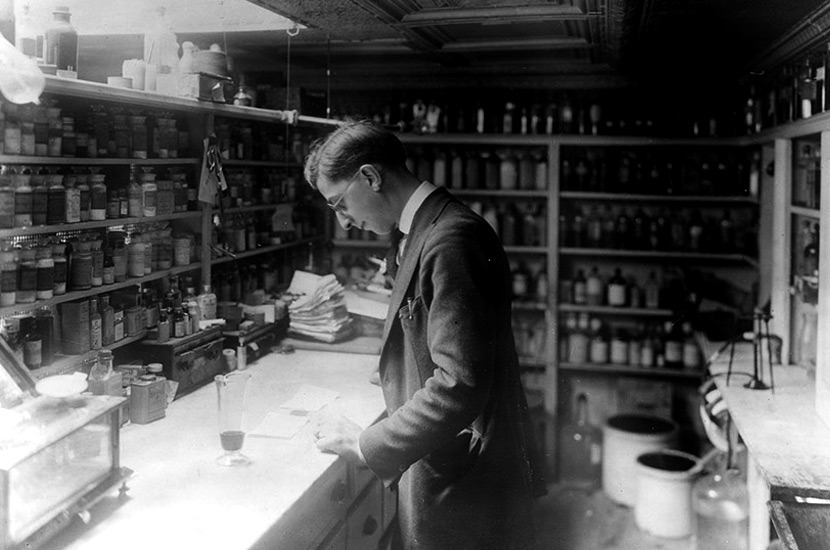
During the pandemic, people in Washington, DC, flocked to pharmacies, like People’s Drug Store No. 5, to buy medications in search of a cure for influenza.
20. Red Cross Volunteers – Detroit, MI

In Detroit, Red Cross volunteers, including the Motor Corps and Canteen groups, delivered supplies to flu victims. The Red Cross worked with the Department of Health to visit homes, prepare food, and care for children.
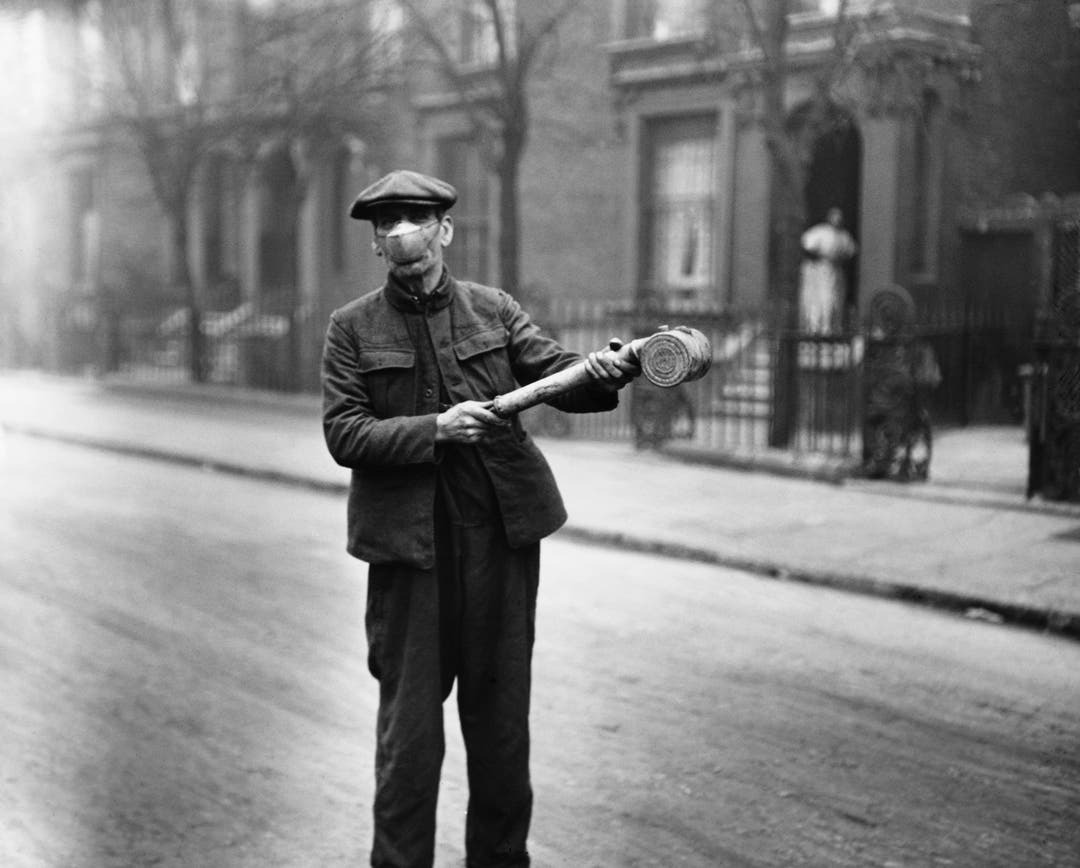
21. Street Sweeper – New York, NY
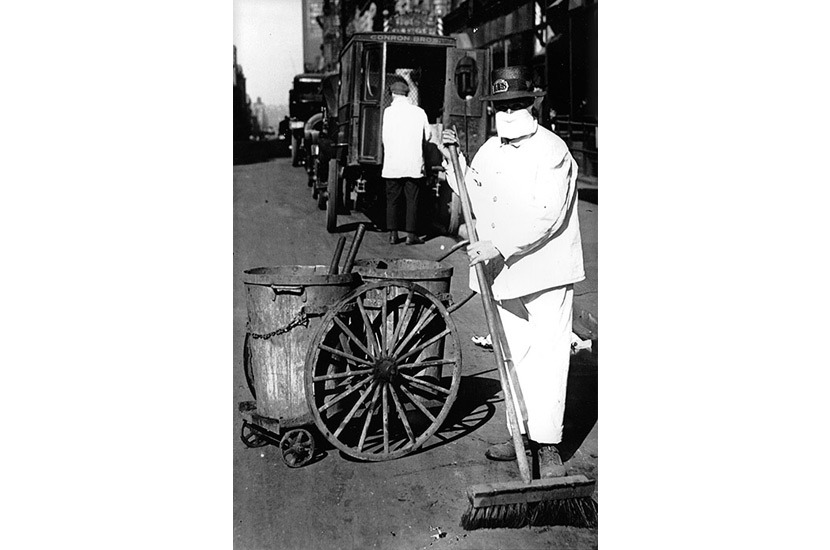
In New York City, a street sweeper wears a mask while working in October 1918. Some street sweepers were also recruited as gravediggers to help bury flu victims.
22. Open-air Police Court – San Francisco, CA

As flu cases surged in San Francisco, judges held court outdoors to avoid crowding. The city’s Board of Health recommended people avoid crowded places and streetcars and suggested holding events outdoors or canceling them altogether.
23. Ambulance Duty – St. Louis, MO

The Red Cross Motor Corps in St. Louis provided ambulance services during the epidemic. They recruited volunteers and drivers to transport nurses to quarantined homes. About 40 nurses cared for around 3,000 patients who couldn’t access private care.
24. St. Louis Red Cross Motor Corps on duty during the 1918 flu epidemic

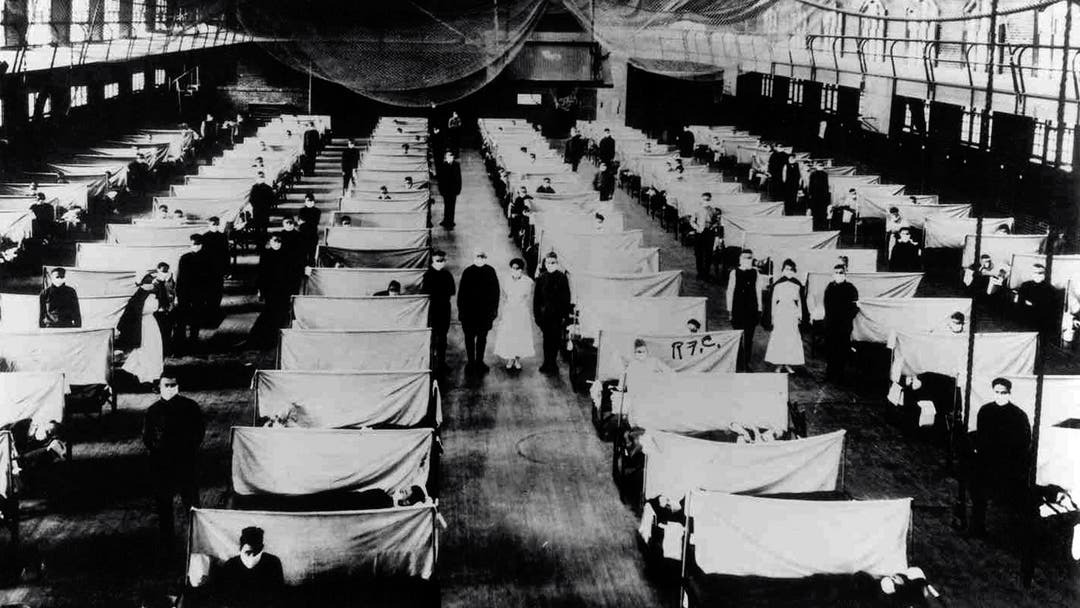
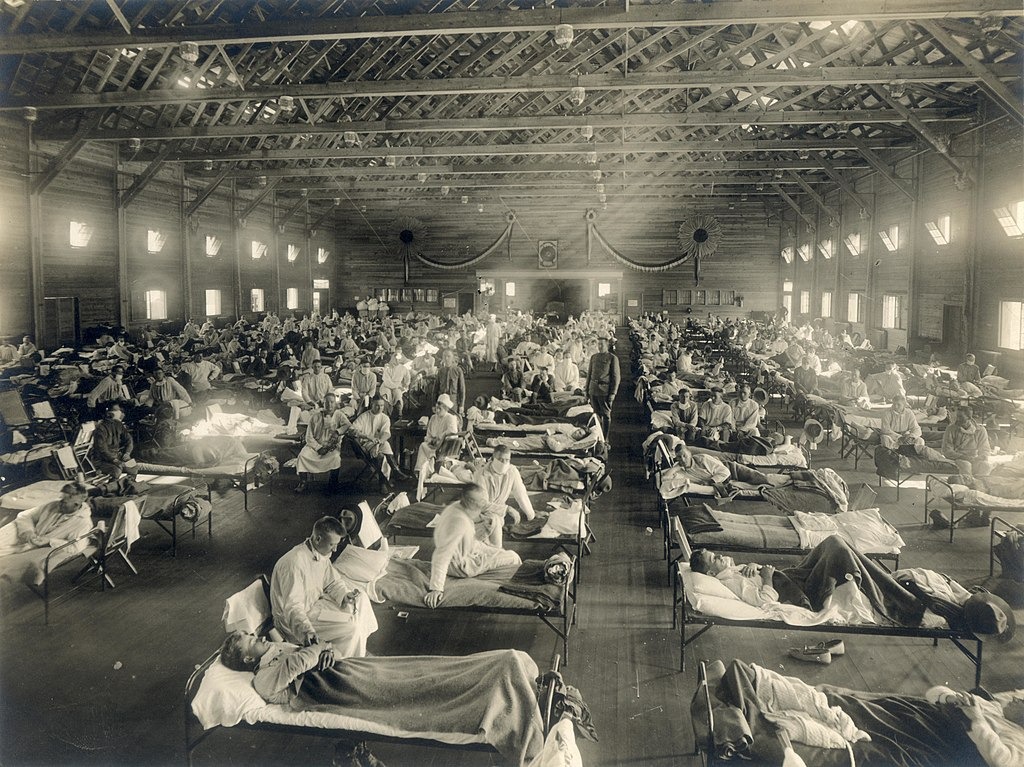
25. Soldiers sick with Spanish flu at a hospital ward at Camp Funston in Fort Riley, Kansas
26. Seattle policemen wearing cloth face masks handed out by the American Red Cross during the Spanish flu pandemic, December 1918

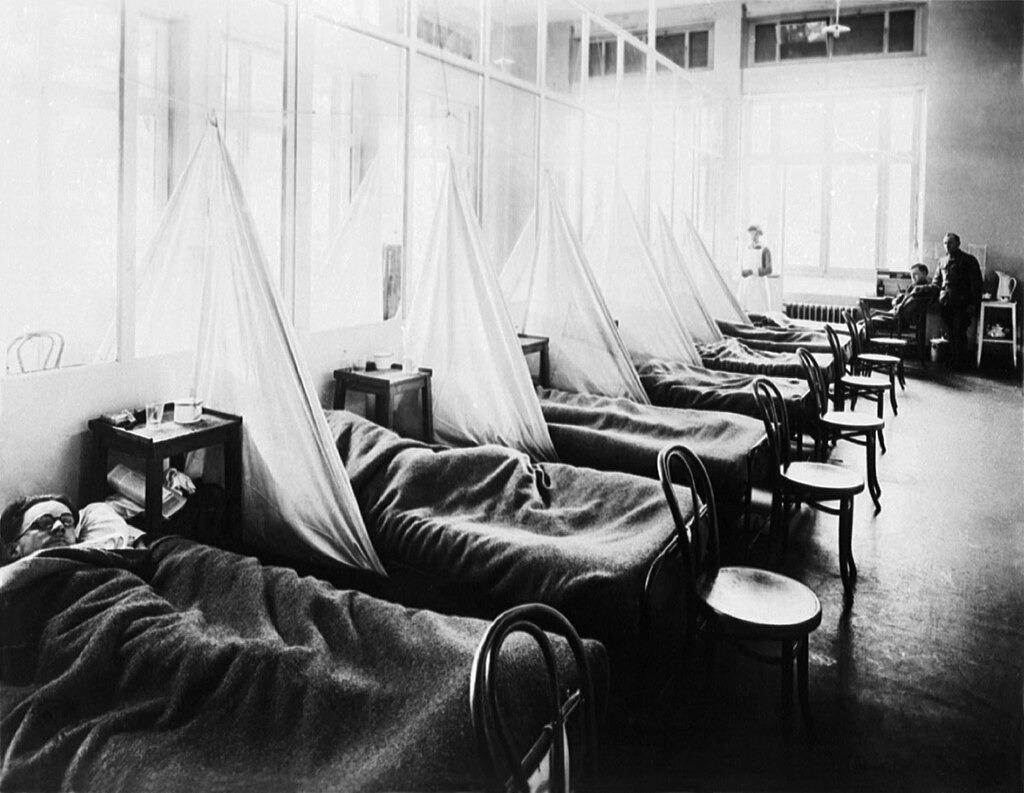
27. American Expeditionary Force flu patients at U.S. Army Camp Hospital no. 45 in Aix-les-Bains, France, 1918
28. Public health recommendations from the Illustrated Current News
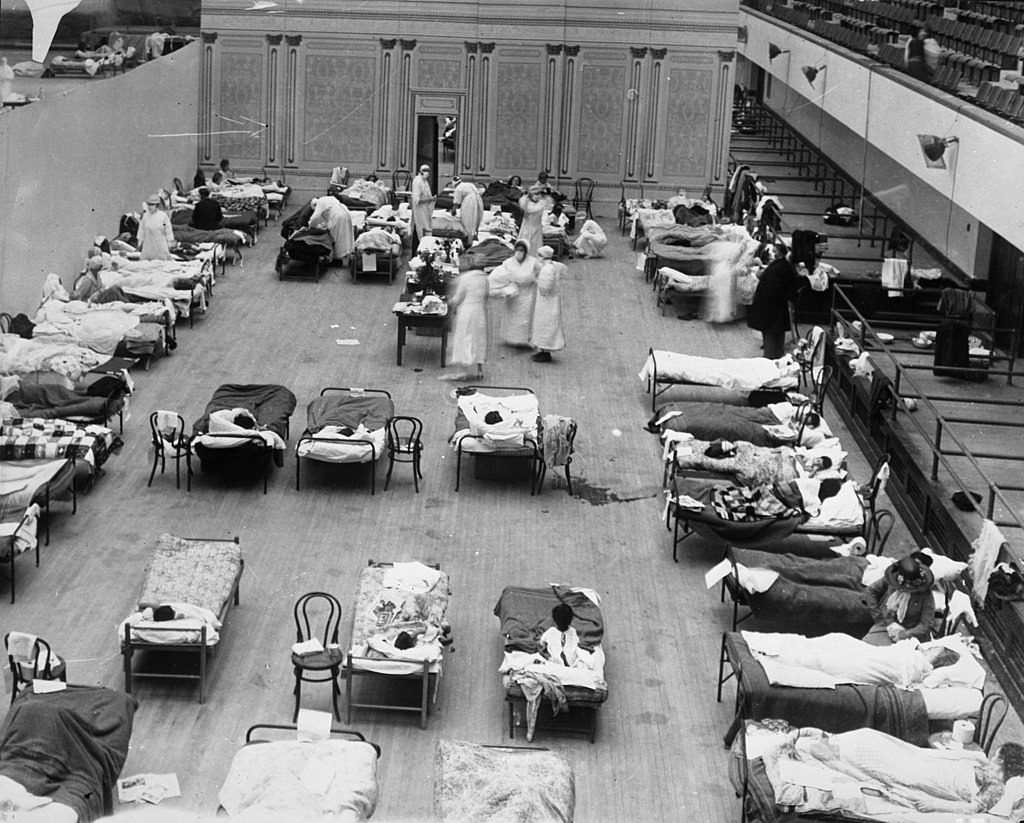
29. American Red Cross nurses tend to flu patients in temporary wards set up inside the Oakland Municipal Auditorium
30. U.S. Army flu patients at Field Hospital No. 29 near Hollerich, Luxembourg 1918. As U.S. troops deployed en masse for the war effort in Europe, they carried the Spanish flu with them.
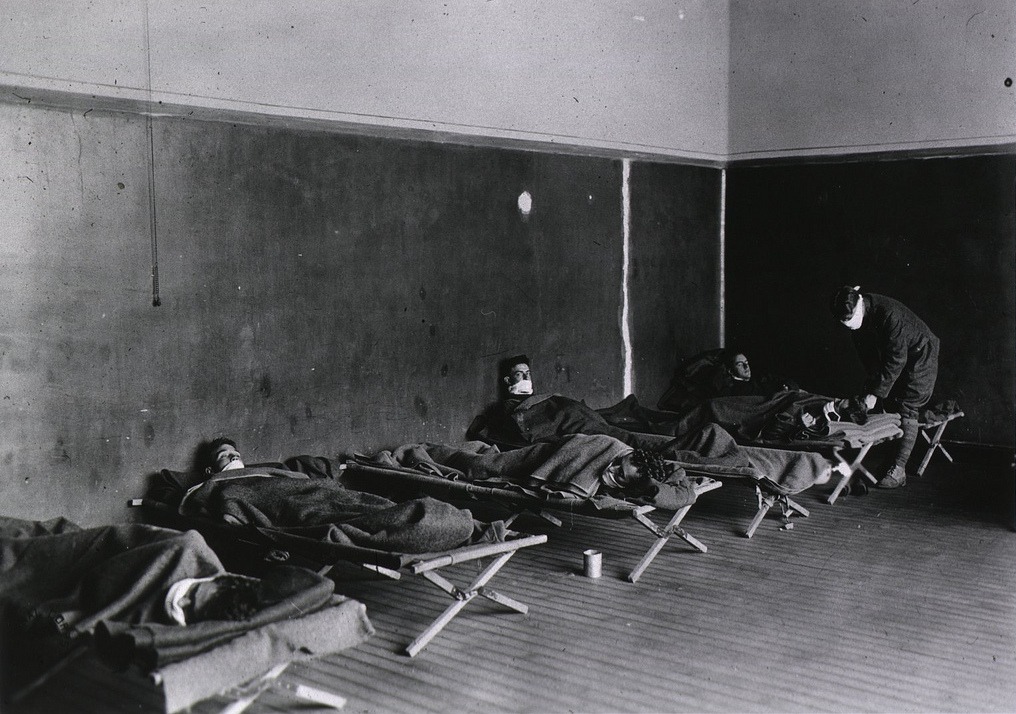
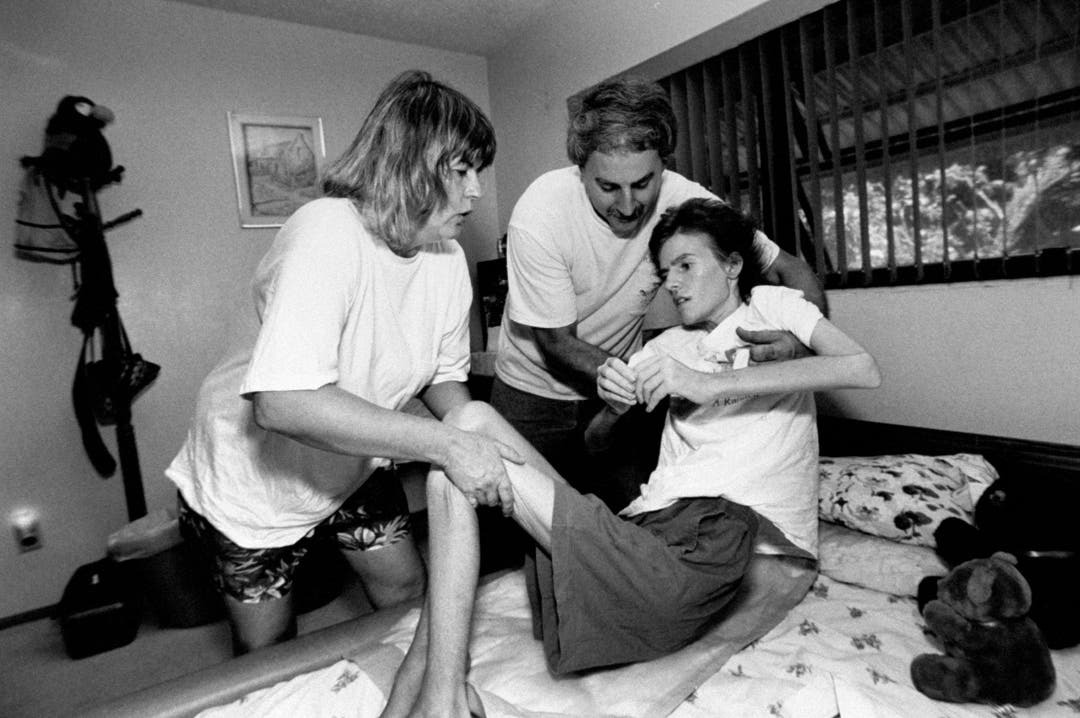
31. A nurse wears a cloth face mask while treating a flu patient in Washington, DC, c. 1919

32. A hospital during the 1918 flu pandemic

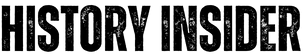
33. Dr Terrence Tumpey examines a reconstructed version of the Spanish flu virus at the CDC